Quantitative, structural and molecular changes in neuroglia of aging mammals: A review
Accepted: 27 May 2021
HTML: 10
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
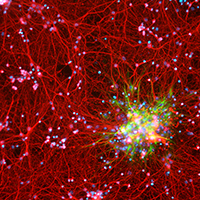
The neuroglia of the central and peripheral nervous systems undergo numerous changes during normal aging. Astrocytes become hypertrophic and accumulate intermediate filaments. Oligodendrocytes and Schwann cells undergo alterations that are often accompanied by degenerative changes to the myelin sheath. In microglia, proliferation in response to injury, motility of cell processes, ability to migrate to sites of neural injury, and phagocytic and autophagic capabilities are reduced. In sensory ganglia, the number and extent of gaps between perineuronal satellite cells – that leave the surfaces of sensory ganglion neurons directly exposed to basal lamina– increase significantly. The molecular profiles of neuroglia also change in old age, which, in view of the interactions between neurons and neuroglia, have negative consequences for important physiological processes in the nervous system. Since neuroglia actively participate in numerous nervous system processes, it is likely that not only neurons but also neuroglia will prove to be useful targets for interventions to prevent, reverse or slow the behavioral changes and cognitive decline that often accompany senescence.
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2021.3249
https://doi.org/10.4081/ejh.2021.3249






