Mucin1 relieves acute lung injury by inhibiting inflammation and oxidative stress
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 16 November 2021
Authors
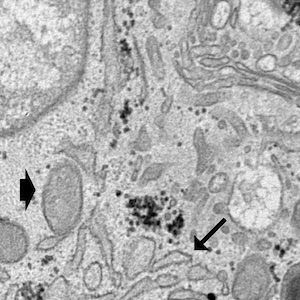
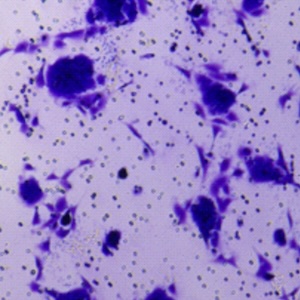
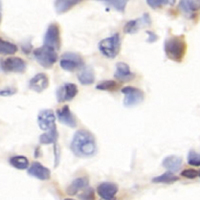
Acute lung injury/acute respiratory distress syndrome (ALI/ARDS) is a kind of diffuse inflammatory injury caused by various factors, characterized by respiratory distress and progressive hypoxemia. It is a common clinical critical illness. The aim of this study was to investigate the effect and mechanism of the Mucin1 (MUC1) gene and its recombinant protein on lipopolysaccharide (LPS)-induced ALI/ARDS. We cultured human alveolar epithelial cell line (BEAS-2B) and used MUC1 overexpression lentivirus to detect the effect of MUC1 gene on BEAS-2B cells. In addition, we used LPS to induce ALI/ARDS in C57/BL6 mice and use hematoxylin and eosin (H&E) staining to verify the effect of their modeling. Recombinant MUC1 protein was injected subcutaneously into mice. We examined the effect of MUC1 on ALI/ARDS in mice by detecting the expression of inflammatory factors and oxidative stress molecules in mouse lung tissue, bronchoalveolar lavage fluid (BALF) and serum. Overexpression of MUC1 effectively ameliorated LPS-induced damage to BEAS-2B cells. Results of H&E staining indicate that LPS successfully induced ALI/ARDS in mice and MUC1 attenuated lung injury. MUC1 also reduced the expression of inflammatory factors (IL-1β, TNF-α, IL-6 and IL-8) and oxidative stress levels in mice. In addition, LPS results in an increase in the activity of the TLR4/NF-κB signaling pathway in mice, whereas MUC1 decreased the expression of the TLR4/NF-κB signaling pathway. MUC1 inhibited the activity of TLR4/NF-κB signaling pathway and reduced the level of inflammation and oxidative stress in lung tissue of ALI mice.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.