Senescence-associated ß-galactosidase staining over the lifespan differs in a short- and a long-lived fish species
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 21 February 2024
Authors
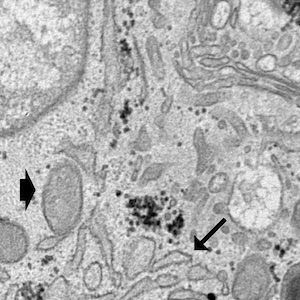
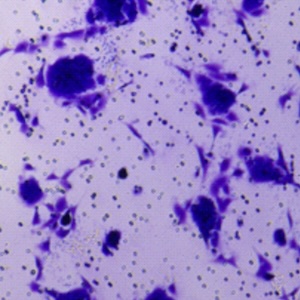
During the aging process, cells can enter cellular senescence, a state in which cells leave the cell cycle but remain viable. This mechanism is thought to protect tissues from propagation of damaged cells and the number of senescent cells has been shown to increase with age. The speed of aging determines the lifespan of a species and it varies significantly in different species. To assess the progress of cellular senescence during lifetime, we performed a comparative longitudinal study using histochemical detection of the senescence-associated beta-galactosidase as senescence marker to map the staining patterns in organs of the long-lived zebrafish and the short-lived turquoise killifish using light- and electron microscopy. We compared age stages corresponding to human stages of newborn, childhood, adolescence, adult and old age. We found tissue-specific but conserved signal patterns with respect to organ distribution. However, we found dramatic differences in the onset of tissue staining. The stained zebrafish organs show little to no signal at newborn age followed by a gradual increase in signal intensity, whereas the organs of the short-lived killifish show an early onset of staining already at newborn stage, which remains conspicuous at all age stages. The most prominent signal was found in liver, intestine, kidney and heart, with the latter showing the most prominent interspecies divergence in onset of staining and in staining intensity. In addition, we found staining predominantly in epithelial cells, some of which are post-mitotic, such as the intestinal epithelial lining. We hypothesize that the association of the strong and early-onset signal pattern in the short-lived killifish is consistent with a protective mechanism in a fast growing species. Furthermore, we believe that staining in post-mitotic cells may play a role in maintaining tissue integrity, suggesting different roles for cellular senescence during life.
Ethics Approval
The animal experiment was approved by the Austrian Federal Ministry of Education, Science and ResearchSupporting Agencies
Austrian Science Fund (FWF)/Herzfelder’sche FamilienstiftungHow to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.