Endoplasmic reticulum stress contributed to inflammatory bowel disease by activating p38 MAPK pathway
Accepted: 16 May 2022
HTML: 36
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
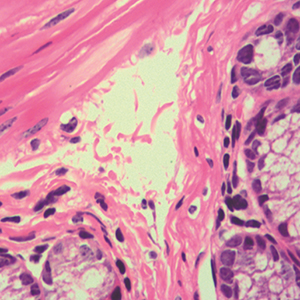
Recent evidence suggests that endoplasmic reticulum (ER) stress plays a vital role in inflammatory bowel disease (IBD). Therefore, the aim of this study was to investigate the mechanism by which ER stress promotes inflammatory response in IBD. The expression of Gro-α, IL-8 and ER stress indicator Grp78 in colon tissues from patients with Crohn’s disease (CD) and colonic carcinoma was analyzed by immunohistochemistry staining. Colitis mouse model was established by the induction of trinitrobenzene sulphonic acid (TNBS), and the mice were treated with ER stress inhibitor tauroursodeoxycholic acid (TUDCA). Then the body weight, colon length and colon inflammation were evaluated, and Grp78 and Gro-α in colon tissues were detected by immunohistochemistry. Epithelial cells of colon cancer HCT116 cells were treated with tunicamycin to induce ER stress. Grp78 was detected by Western blot, and chemokines were measured by PCR and ELISA. The expression levels of Grp78, Gro-α and IL-8 were significantly upregulated in intestinal tissues of CD patients. Mice with TNBS induced colitis had increased expression of Grp78 and Gro-α in colonic epithelia. TUDCA reduced the severity of TNBS-induced colitis. In HCT116 cells, tunicamycin increased the expression of Grp78, Gro-α and IL-8 in a concentration-dependent manner. Furthermore, p38 MAPK inhibitor significantly inhibited the upregulation of Gro-α and IL-8 induced by tunicamycin. In conclusion, ER stress promotes inflammatory response in IBD, and the effects may be mediated by the activation of p38 MAPK signaling pathway.
Ethics Approval
All animal experiments were reviewed and approved by the Institutional Animal Care Committee of Changsha Central Hospital (Approval No. 20200512)Rights
Natural Science foundation of Hunan Province of China (No. 2019JJ40319), Project of Hunan Province, Department of Health (No. B2019142), Project of Changsha Science and Technology Bureau (No. kq2004167), and Hunan Science and Technology Innovation Plan Project (No. 2020SK53306)How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2022.3415
https://doi.org/10.4081/ejh.2022.3415






