LINC00926 is involved in hypoxia-induced vascular endothelial cell dysfunction via miR-3194-5p regulating JAK1/STAT3 signaling pathway
Accepted: 29 December 2022
HTML: 28
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
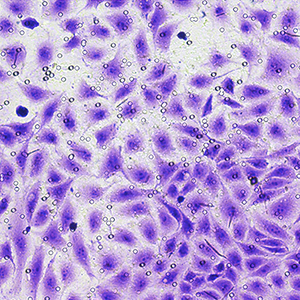
Vascular endothelial cell (VEC) dysfunction is associated with the development of coronary heart disease (CHD). Long intergenic non-protein coding RNA 926 (LINC00926), a kind of long noncoding RNA (lncRNA), has been found to be abnormally expressed in CHD patients. However, the biological role of LINC00926 has not been reported. In our research, we intended to explore the regulatory mechanism of LINC00926 in hypoxia-exposed HUVEC cells (HUVECs). In our in vitro study, HUVECs were exposed under hypoxic conditions (5% O2) for 24 h. RT-qPCR and Western blotting assay were used to detect the mRNA and protein levels. CCK-8 assay, flow cytometry, transwell assay and in vitro angiogenesis assay were performed to measure cell proliferation, apoptosis, migration and tube formation, respectively. Bioinformatics analysis was applied to predict the target of LINC00926 and miR-3194-5p, which was verified by dual-luciferase reporter assays. The results showed that LINC00926 was highly expressed in CHD patients and hypoxia-exposed HUVECs. LINC00926 overexpression suppressed cell proliferation, migration and tube formation and increased cell apoptosis. MiR-3194-5p was a target of LINC00926 and can target binding to JAK1 3’UTR. LINC00926 could up-regulate JAK1 and p-STAT3 levels via miR-3194-5p. In addition, overexpressed LINC00926 suppressed cell proliferation, migration and tube formation and increased cell apoptosis via miR-3194-5p/JAK1/STAT3 axis. In summary, LINC00926 aggravated endothelial cell dysfunction via miR-3194-5p regulating JAK1/STAT3 signaling pathway in hypoxia-exposed HUVECs.
Ethics Approval
This study was approved by the Ethics Committee of Jilin Medical UniversityHow to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2023.3526
https://doi.org/10.4081/ejh.2023.3526






