Curculigoside inhibits osteoarthritis via the regulation of NLRP3 pathway
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 27 November 2023
Authors
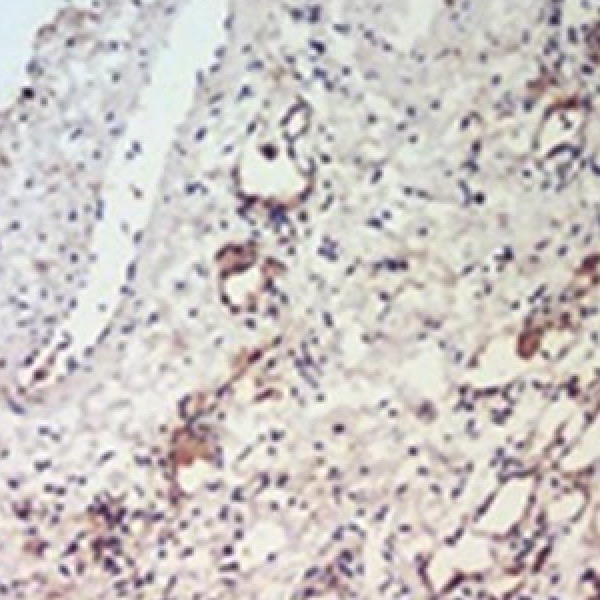
Osteoarthritis (OA) is characterized by degenerative articular cartilage. Nucleotide-binding oligomerization domain-like receptor containing pyrin domain 3 (NLRP3) plays an important role in inflammation. This study aims to investigate whether protective effects of curculigoside on OA are medicated by the regulation of NLRP3 pathway. Destabilization of the medial meniscus (DMM) was performed to build an OA mouse model. After surgery, OA mice were treated with curculigoside. Immunohistochemistry was conducted to evaluate OA cartilage. In addition, human chondrocytes were isolated and treated with curculigoside. The mRNA and protein expression of iNOS, MMP-9, NLRP3 was detected by PCR and Western blot analysis. Curculigoside inhibited mRNA and protein levels of iNOS and MMP-9 induced by DMM surgery in a dose-dependent manner. Furthermore, the expression of NLRP3, NF-κB and PKR was downregulated after curculigoside administration. Moreover, curculigoside reversed the effects of IL-1β on MMP-9, iNOS and type II collagen expression at mRNA and protein levels in human chondrocytes in a dose-dependent manner. In conclusion, curculigoside exhibits beneficial effect on cartilage via the inhibition of NLRP3 pathway.
Ethics Approval
this study was approved by the Ethics Committee of Shanxi Bethune Hospital, All animal study protocols were approved by the Animal Care and Use Committee of Shanxi Bethune HospitalHow to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.









