NOP14 regulates the growth, migration, and invasion of colorectal cancer cells by modulating the NRIP1/GSK-3β/β-catenin signaling pathway
Accepted: 25 May 2021
HTML: 25
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
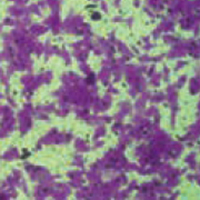
Colorectal cancer (CRC) is the third most common cancer diagnosed worldwide. Recently, nucleolar complex protein 14 (NOP14) has been discovered to play a critical role in cancer development and progression, but the mechanisms of action of NOP14 in colorectal cancer remain to be elucidated. In this study, we used collected colorectal cancer tissues and cultured colorectal cancer cell lines (SW480, HT29, HCT116, DLD1, Lovo), and measured the mRNA and protein expression levels of NOP14 in colorectal cancer cells using qPCR and western blotting. GFP-NOP14 was constructed and siRNA fragments against NOP14 were synthesized to investigate the importance of NOP14 for the development of colorectal cells. Transwell migration assays were used to measure cell invasion and migration, CCK-8 kits were used to measure cell activity, and flow cytometry was applied to the observation of apoptosis. We found that both the mRNA and protein levels of NOP14 were significantly upregulated in CRC tissues and cell lines. Overexpression of GFP-NOP14 markedly promoted the growth, migration, and invasion of the CRC cells HT19 and SW480, while genetic knockdown of NOP14 inhibited these behaviors. Overexpression of NOP14 promoted the expression of NRIP1 and phosphorylated inactivation of GSK-3β, leading to the upregulation of β-catenin. Genetic knockdown of NOP14 had the opposite effect on NRIP1/GSK-3/β-catenin signals. NOP14 therefore appears to be overexpressed in clinical samples and cell lines of colorectal cancer, and promotes the proliferation, growth, and metastasis of colorectal cancer cells by modulating the NRIP1/GSK-3β/β-catenin signaling pathway.
Present address: School of Medicine, Southeast University, Nanjing, China
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2021.3246
https://doi.org/10.4081/ejh.2021.3246






