PD-L1 expression with QR1 and E1L3N antibodies according to histological ovarian cancer subtype: A series of 232 cases
Accepted: 10 February 2021
HTML: 12
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Authors
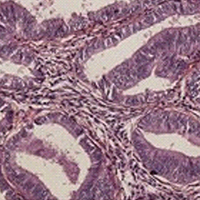
Therapeutic strategies for epithelial ovarian cancers are evolving with the advent of immunotherapy, such as PD-L1 inhibitors, with encouraging results. However, little data are available on PDL-1 expression in ovarian cancers. Thus, we set out to determine the PD-L1 expression according to histological subtype. We evaluated the expression of two PD-L1 clones – QR1 and E1L3N – with two scores, one based on the percentage of labeled tumor cells (tumor proportion score, TPS) and the other on labeled immune cells (combined proportion score, CPS) in a consecutive retrospective series of 232 ovarian cancers. PD-L1 expression was more frequent in high grade serous carcinoma (27.5% with E1L3N clone and 41.5% with QR1 clone), grade 3 endometrioid carcinoma (25% with E1L3N clone and 50% with QR1 clone), and clear-cell carcinomas (27.3% with E1L3N clone and 29.6% with QR1 clone) than other histological subtypes with CPS score. Using the CPS score, 17% of cases were labeled with E1L3N vs 28% with QR1. Using the TPS score, 14% of cases were positive to E1L3N vs 17% for QR1. For TPS and CPS, respectively, 77% and 78% of the QR1 cases were concordant with E1L3N for the thresholds of 1%. Overall and progression-free survival between PD-L1 positive and PD-L1 negative patients were not different across all histological types, and each subtype in particular for serous carcinomas expressing PD-L1. Expression of PD-L1 is relatively uncommon in epithelium ovarian tumors. When positive, usually <10% of tumor cells are labeled. QR1 clone and CPS appear the best tools to evaluate PD-L1 expression.
Ethics Approval
The study was approved by the Ethics Committee “Comité d’éthique de la recherche en Obstétrique et Gynécologie (CEROG)” (number CEROG 2019-GYN-1102 “phenotypic profiles identified in epithelial ovarian cancers”)UMR_S938, Sorbonne University, Hôpital Saint Antoine, Sorbonne Université, Paris
UMR_S938, Sorbonne University, Hôpital Saint Antoine, Sorbonne Université, Paris; Clinical Research Group (GRC6-Sorbonne Université) Endometriosis expert center, C3E, Paris
UMR_S938, Sorbonne University, Hôpital Saint Antoine, Sorbonne Université, Paris; Clinical Research Group (GRC6-Sorbonne Université) Endometriosis expert center, C3E, Paris
How to Cite
PAGEPress has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.

 https://doi.org/10.4081/ejh.2021.3185
https://doi.org/10.4081/ejh.2021.3185






