The lncRNA MEG3 promotes trophoblastic cell growth and invasiveness in preeclampsia by acting as a sponge for miR-21, which regulates BMPR2 levels
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Accepted: 19 October 2021
Authors
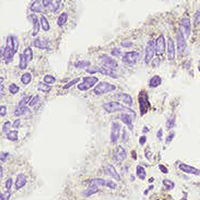
Preeclampsia (PE) is one of the leading causes of maternal morbidity and mortality in pregnant women. This study aimed to investigate the potential impact and regulatory mechanisms of bone morphogenetic protein receptor 2 (BMPR2) on the progression of PE. We obtained placental tissues from pregnant women with PE and normal pregnant women, and the results showed that BMPR2 was expressed at low levels in the tissue from PE women. Genetic knockdown of BMPR2 increased the proliferation and invasion of cultured trophoblast cells, whereas its overexpression reduced these characteristics. Bioinformatics analysis and luciferase reporter gene assays confirmed that BMPR2 is a direct target of miR-21. Overexpression of a miR-21 inhibitor promoted the growth and invasiveness of trophoblast cells, whereas the opposite results were observed for the miR-21 mimic. Furthermore, miR-21 was sponged by the lncRNA MEG3, and shRNA inhibition of MEG3 reduced trophoblast cell growth and invasiveness. miR-21 was upregulated in the tissues from PE women, whereas MEG3 was downregulated, and the two were negatively correlated. Collectively, this study demonstrates that the lncRNA MEG3 acts as a sponge for miR-21, which regulates BMPR2 expression and promotes trophoblast cell proliferation and invasiveness, thereby preventing the development of PE. These findings provide novel insight into a targeted therapy that could be used to treat or prevent the development of PE.
Department of Obstetrics and Gynecology, Zhongshan People's Hospital Zhongshan Hospital of Sun Yat-sen University, Zhongshan
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.









