Tanshinone IIA attenuates hepatic stellate cell activation, oxidative stress, and liver fibrosis by inhibiting YAP signaling

All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
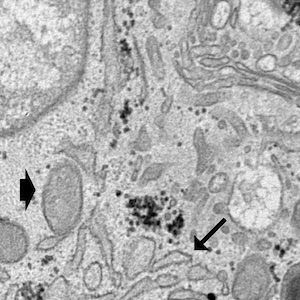
Authors
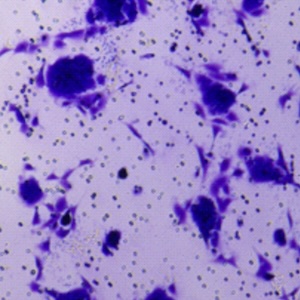
Tanshinone IIA is derived from Salvia miltiorrhiza and has multiple therapeutic targets and functions. The exact therapeutic effects on liver fibrosis as well as the underlying hepatoprotective mechanisms are still lacking. A liver fibrosis model was established via ligation of the common bile duct ligation (BDL). The mice were intraperitoneally administered different concentrations of tanshinone IIA (4 mg/kg, 8 mg/kg) for 2 weeks. Liver function was assessed through hematoxylin and eosin and Sirus red staining. Serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), glutathione (GSH) and malondialdehyde (MDA) were quantified by enzyme-linked immunosorbent assay (ELISA), via microplate reader. The total iron content of the liver was quantified via Triple Quad-ICP-MS. TGFβ-induced hepatic stellate cells (HSCs), a cell model of liver fibrosis, were treated with tanshinone IIA at different concentrations (10 mM, 20 mM, 30 mM, 40 mM). The combination of tanshinone IIA with YAP agonists was applied in activated HSCs and animal models. Tanshinone IIA treatment relieved BDL-induced liver fibrosis; mitigated histological liver damage; lowered the serum ALT and AST levels; reduced macrophage infiltration and the MDA and iron contents; and increased the GSH and GPX4 levels by inhibiting YAP signaling. tanshinone IIA also suppressed the activation of HSCs and collagen production through blocking the YAP signaling pathway. The YAP agonist reversed the therapeutic effect of tanshinone IIA on activated HSCs and BDL-induced liver fibrosis. Tanshinone IIA inhibited HSC activation and oxidative stress and alleviated liver fibrosis by inhibiting the YAP signaling pathway.
How to Cite

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.